Many women who have had a myomectomy are told that a vaginal birth just isn’t an option. Often, that message comes without a conversation about what kind of myomectomy they had, what the evidence says or what type of birth experience the woman actually wants.
At The VBAC Link, we believe parents deserve clear information, honest conversations and the chance to make informed decisions. That’s why it’s so important to us to share vaginal birth after myomectomy (VBAM) stories like Mabel’s (Episode 189) and Magdalena’s (Episode 442).
What Are Fibroids?
Fibroids (uterine leiomyomas) are non-cancerous growths that develop in or on the uterus.
They are incredibly common:
- Up to 70–80% of women will develop fibroids by age 50
- Many have no symptoms at all
- Others experience heavy bleeding, pain, pressure or fertility challenges
Fibroids vary widely in size, number and location, which is why treatment and future birth planning are never universally the same for everyone.
What Is a Myomectomy?
A myomectomy is a surgical procedure to remove fibroids while preserving the uterus. It’s often chosen by people who want relief from symptoms and hope to become pregnant or carry future pregnancies.
Myomectomy is one of the most common gynecologic surgeries. And because the uterus remains intact, vaginal birth can still be possible afterward.
Does the Type of Myomectomy Matter?
Yes. The details of the surgery matter far more than the word “myomectomy.”
Hysteroscopic Myomectomy
- Fibroids removed through the cervix
- No incision into the uterine muscle
- Does not increase uterine rupture risk
- Often treated like an unscarred uterus in labor
Laparoscopic or Robotic Myomectomy
- Small abdominal incisions
- Fibroids removed from the uterine wall
- Risk depends on
- Depth of incisions
- Number of fibroids removed
- Whether the uterine cavity was entered
Many people with this history go on to have vaginal births.
Open (Abdominal) Myomectomy
- Larger incision, similar to a Cesarean
- Often used for large or multiple fibroids
- Historically approached with more caution, but evidence still shows
- Low absolute risk of uterine rupture
- VBAM can be an option for some with individualized care
What Are the Real Risks After Myomectomy?
Uterine Rupture
Research shows:
- Overall uterine rupture risk after myomectomy is under 1%
- During a trial of labor, rates are around 0.4–0.5%
- Many ruptures reported in studies occurred before labor, not during it.
Learn more about general uterine rupture rates in VBAC here.
Placenta Previa
Women with a myomectomy history also had higher odds of placenta previa compared to those without fibroids.
VBAM Rates
In a pooled review of multiple studies (3,685 pregnancies total):
Among those who labored after laparoscopic myomectomy:
- 93% had a vaginal birth
- 7% ended in cesarean after laboring (secondary cesarean).
After open (abdominal) myomectomy:
- 88% delivered vaginally
- 12% required cesarean after laboring
What These Stats Don’t Show
Numbers alone don’t tell the whole story. Many factors influence outcomes after myomectomy, including
- Surgical details: how many fibroids were removed, whether the uterine cavity was entered, and where incisions were placed
- Type of surgery: laparoscopic vs open myomectomy
- Timing of conception after surgery
- Provider and hospital policies
- Individual health variables
That’s why decisions about VBAM should always be individualized.
Risks of Cesarean Birth After Myomectomy
While cesarean birth can be lifesaving, scheduling a cesarean after a prior myomectomy means adding another uterine scar, which comes with risks.
- Placenta accreta spectrum (PAS) in future pregnancies
Occurs in approximately 0.96% of pregnancies after myomectomy. Risk increases further with cesarean delivery. - Increased surgical complexity
Cesareans after myomectomy are associated with more adhesions, longer operative times, and greater blood loss due to scar tissue and altered uterine anatomy. - Postpartum hemorrhage (PPH)
PPH occurs in approximately3–6% of cesarean births overall, with prior uterine surgery identified as a contributing risk factor. - Infection risk
Endometritis or surgical site infection occurs in about 2–7% of cesarean births, with higher rates in repeat or prolonged surgeries. - Bladder or bowel injury
Bladder injury occurs in roughly 0.1–0.5% of primary cesareans and up to 1% in repeat or complex cesareans, with higher risk when adhesions are present after prior uterine surgery.
When weighing VBAM versus planned Cesarean, it’s important to compare the risks of labor and the risks of another surgery, especially for those hoping for more children.
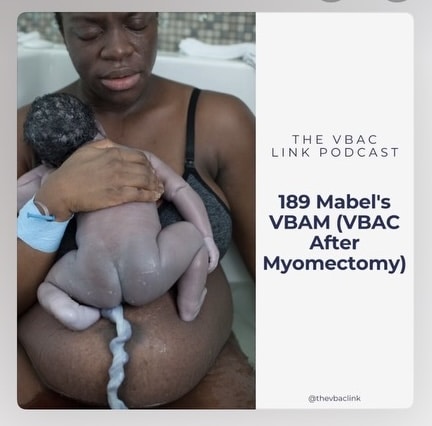
Episode 189: Mabel’s Story
In Episode 189, Mabel shares her journey navigating pregnancy and birth after a myomectomy. She talks openly about being given alarming statistics that didn’t match the research and how learning the evidence changed her confidence and decision-making.
Mabel’s story made big waves in our community. It became a lifeline for others.
Episode 442: Magdalena Heard the Story—and Reached Out
In Episode 442, Magdalena explains how listening to Mabel’s episode changed everything for her.
“One doctor told me I had a 9% chance of rupture. When I looked at the research Mabel shared with me, the true number was under 1%.”
That moment mattered. Magdalena reached out to Mabel, dove into the research, and began preparing for a VBAM that felt informed and empowering.
Magdalena’s VBAM Preparation (In Her Own Words)
Magdalena shared these reflections to help others considering VBAM. A gentle reminder that this is her personal experience, not medical advice.
1. Get Your Surgical Notes
“Read them carefully to see whether the uterine cavity was breached or if any fundal fibroids were removed. Providers also tend to be more supportive of laparoscopic myomectomies.”
2. Find VBAC-Friendly Care
“Find a VBAC-friendly provider. They’re far more likely to support a VBAM.”
She also emphasized choosing VBAC-friendly hospitals where practices like delayed cord clamping and immediate skin-to-skin are standard even during cesareans.
3. Consider a Doula
“A doula can help with research, provider selection, and navigating hospitals—especially if they’re familiar with the staff and environment.”
4. Be Intentional About Induction
“I declined any form of induction and was comfortable going past my due date, even with my ‘big’ babies.”
She chose to avoid Pitocin because:
“It felt important to be able to sense if something didn’t feel right.”
5. Understand Your Pain-Relief Options
“Low-dose epidurals can allow movement and sensation. I’ve also heard of providers turning off the epidural for pushing so you can feel your contractions.”
6. Community and Education Matter
“Podcasts were a huge part of my preparation. The only VBAM-specific one I found was The VBAC Link.”
She also found support in:
- Special Scars – Special Hope (Facebook group)
- The VBAC Link Community
- Local birth groups in her country
7. Do the Research, and Bring It With You
“Print it, highlight it, and share it with your provider. The more informed you are, the less likely you’ll be talked into unnecessary interventions.”
Magdalena’s Second Birth Preparation
Magdalena also shared how her mental, emotional, and spiritual preparation with her second VBAM played a HUGE role in making it an even more empowering experience than her first:
- Revisited the Pain Free Birth course
- Read Ina May’s Guide to Childbirth
- Attended a retreat with meditation, yoga, and deep rest
- Completed a 40-day Christian forgiveness course
- Practiced meditation and breathwork (including Joe Dispenza techniques)
- Attended women’s circles, cacao ceremonies, and yin yoga
- Stopped working nearly a month before her due date
- Switched to walking and yoga after 34 weeks
- Received frequent massages
“During labor, I went into the most amazing full-body shivers. I genuinely enjoyed transition. I surrendered completely—and I loved it.”
Research & References (VBAM / TOLAM)
These are the studies Mabel shared with Magdalena and that support current discussions around VBAM:
- Trial of labor after myomectomy and uterine rupture – systematic review
- Vaginal birth after prior myomectomy
- Pregnancy outcomes after myomectomy
- Guidelines on pregnancy after myomectomy
- Risk of uterine rupture after myomectomy
What These Stories Teach Us
- Fibroids & myomectomy are common
- VBAM is not automatically unsafe or impossible
- Risk exists, but it is low, measurable and personal
- Information changes confidence
- Community changes outcomes
At The VBAC Link, while we can’t promise a specific birth outcome, we do believe you deserve information, respect and choice.
A special thank you to our sweet friend, Mags, who shared all of this wisdom and her resources with us today. Our community is just the best, and this is why.
We love you and are cheering for you, Women of Strength.















 Postpartum Tips for the Holidays: Surviving (and maybe even enjoying) the Season
Postpartum Tips for the Holidays: Surviving (and maybe even enjoying) the Season